Introduction
Human skin exhibits a rich diversity of color and tone, primarily determined by the quantity and distribution of melanin within the epidermis. Melanin plays a crucial protective role against ultraviolet radiation (UVR) damage. However, the increased melanin content in darker skin, while offering photoprotection, can also predispose individuals to specific dermatological conditions. Post-inflammatory hyperpigmentation (PIH) is a common concern, particularly in individuals with darker skin tones. This article explores the molecular mechanisms underlying PIH, the factors contributing to its prevalence in dark skin, and the implications for effective skin care strategies aimed at addressing uneven skin tone and skin discoloration.
Understanding Post-Inflammatory Hyperpigmentation
Post-inflammatory hyperpigmentation presents as darkened, often flattened spots on the skin. The color intensity, ranging from brown to black, depends on the extent of skin damage and the individual’s skin tone. This uneven skin tone results from an overproduction and deposition of melanin following skin inflammation. Exposure to excess sun and UVR can exacerbate PIH. Triggers of PIH include inflammatory skin conditions like acne and atopic dermatitis, allergies, injuries, and cosmetic procedures such as chemical peels and laser treatments. While PIH can affect anyone, it is more frequent and severe in individuals with darkly pigmented skin (Fitzpatrick types III-VI). Factors such as reduced use of photoprotection in these populations and exaggerated melanogenesis in response to inflammation, such as acne, contribute to this disparity. Furthermore, both exogenous factors (e.g., certain cosmetics, mechanical injuries) and endogenous factors (e.g., hormonal changes, systemic diseases) can influence the occurrence of PIH.
Molecular Mechanisms of PIH
Inflammation is central to the development of PIH. Inflammation can damage the basal layer of the epidermis, triggering melanocytes to release melanosomes (pigment-containing granules) into surrounding skin cells. These pigment deposits can persist, leading to prolonged skin discoloration.
In epidermal PIH, inflammatory processes release cytokines, chemokines, and reactive oxygen species (ROS), which stimulate melanocyte growth, melanin synthesis, and its transfer to keratinocytes. Key mediators include epidermal growth factor (EGF), interleukins (IL-1, IL-6), tumor necrosis factor (TNF), leukotrienes, prostaglandins, and thromboxane-A2. Epidermal PIH is characterized by increased pigment in the epidermal basal layer, often accompanied by increased expression of melanoma marker antibody (NKI/beteb) and matrix metalloproteinase-2 (MMP-2).
Dermal PIH occurs when damage to the basement membrane and basal keratinocytes leads to excessive melanin release into the dermis. In the upper dermis, pigment is engulfed by macrophages, causing a darkened appearance. Dermal PIH can be prolonged or even permanent. It is characterized by less epidermal pigmentation but increased infiltration of lymphocytes and expression of macrophage marker CD68 and mast/stem cell growth factor receptor c-kit in the dermis.
Predisposition to PIH in Darker Skin
Individuals with darker skin are more prone to PIH. This increased susceptibility is associated with several factors, including a predisposition to inflammation and differences in skin structure and function.
Systemic Inflammation
Studies have shown increased cases of impaired cutaneous vascular and microvascular function in African American individuals compared to European Americans, even in healthy young adults. This is associated with increased oxidative stress, reduced nitric oxide-mediated vasodilation, and impaired scavenging of superoxide radicals. Lower vitamin D levels, common in darker skin, may also play a role. Furthermore, individuals with darker skin may exhibit low-grade chronic inflammation, with elevated levels of circulating pro-inflammatory cytokines such as IL-6 and C-reactive protein (CRP) (Markiewicz et al.).
Molecular and Cellular Differences
Differences in epidermal structure and function also contribute. While epidermal thickness may not differ, 3D skin models reveal differences in epidermal morphology, with more pronounced differentiation and stratification in European skin. Gene expression studies show differences in biomarkers involved in epidermal morphogenesis and lipid/ceramide metabolism. For example, African skin models may show decreased terminal differentiation of keratinocytes.
The dermal-epidermal junction (DEJ) also differs between light and dark skin. Darker skin often has a thicker dermis with more macrophages and fibroblasts. Papillary fibroblasts in darker skin produce higher amounts of signaling molecules like MCP-1, KGF, MMP1, and TIMP-1. The DEJ in African skin may be longer and more convoluted but contain lower levels of basement membrane markers. These structural and functional differences contribute to the increased propensity for PIH and scarring in darker skin.
Hyperpigmentation and Skin Aging
Hyperpigmentation disorders, including PIH, melasma, and solar lentigos (age spots), are often associated with aging. Inflammation plays a key role in these conditions. The pro-inflammatory cytokine IL-6 is associated with both abnormal melanogenesis in PIH and darker skin tones. Chronic low-grade inflammation, common in older adults, is linked to age-related problems. Cellular senescence, a process where cells cease dividing, also contributes. Senescent cells secrete pro-inflammatory molecules as part of the senescence-associated secretory phenotype (SASP). UVR exposure, a major factor in premature skin aging, can induce inflammation and contribute to the accumulation of senescent cells. As shown in
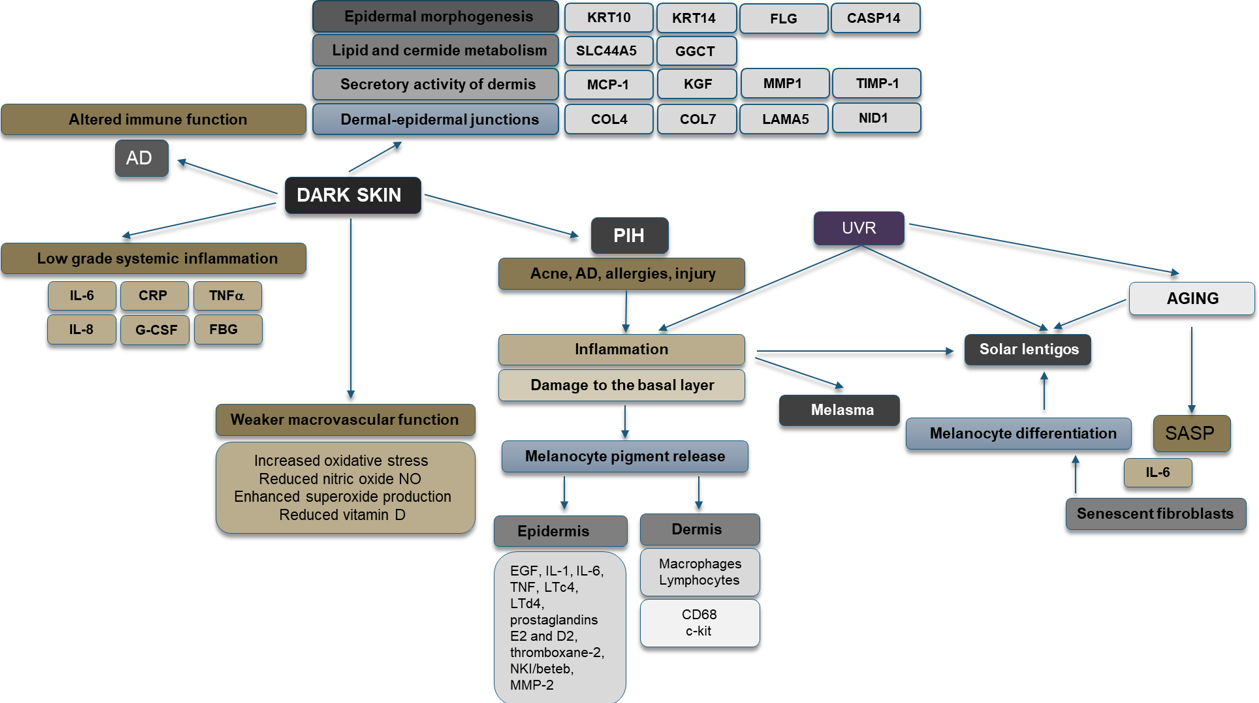
Figure 1, UVR can lead to both PIH and aging via inflammation and cellular senescence.
Current Approaches to Hyperpigmentation Treatment and Skin Care Implications
Current hyperpigmentation treatment options include topical agents and procedures.
Topical Agents:
Many skin care products target hyperpigmentation by reducing melanogenesis and inducing depigmentation. Ingredients include hydroquinone, thiamidol, azelaic acid, kojic acid, arbutin, niacinamide, ellagic acid, and retinoids. Importantly, many of these agents also have anti-inflammatory effects, which can be beneficial in managing PIH. For example, azelaic acid suppresses UVB-induced inflammation, and kojic acid inhibits NF-kB activity.
Procedures:
Chemical peels and laser therapy are also used to treat hyperpigmentation. However, these treatments can trigger inflammation and complications, particularly in darker skin.
Skin Care Implications:
Given the role of inflammation in PIH, skin care strategies should focus on both reducing melanin production and controlling inflammation. For individuals with darker skin, gentle, non-irritating products are essential to minimize inflammation. Broad-spectrum sun protection is crucial to prevent UVR-induced hyperpigmentation and aging. Hyperpigmentation treatment should be tailored to the individual’s skin type and the underlying cause of the PIH.
Conclusion
PIH is a common condition, particularly impacting individuals with darker skin. Its development is influenced by complex interactions between inflammation, cellular processes, and skin structure. Understanding the molecular mechanisms and predisposing factors is crucial for developing effective skin care and hyperpigmentation treatment strategies. Future research should focus on identifying targeted therapies to address PIH and promote even skin tone, especially in individuals with darker skin.
Sources and related content
[1] – Markiewicz, Ewa, et al. “Post-Inflammatory Hyperpigmentation in Dark Skin: Molecular Mechanism and Skincare Implications.” Clinical, Cosmetic and Investigational Dermatology, vol. 15, Dovepress, 25 Nov. 2022, pp. 2555–65. Publications